
S26: EXSTROPHY-EPISPADIAS COMPLEX
Moderators: Rosalia Misseri (USA), Woflgang Rösch (Germany)
ESPU Meeting on Saturday 17, October 2015, 13:35 - 14:35
13:35 - 13:40
S26-1
(LO)
★
LONG-TERM CONTINENCE OUTCOMES IN CLASSIC BLADDER EXSTROPHY
David KEENE, Rachel HARWOOD, A MARIOTTO, Jayne ROBINSON, Janet FISHWICK and Raimondo CERVELLIONE
Royal Manchester Childrens Hospital, Department of Paediatric Urology, Manchester, UNITED KINGDOM
PURPOSE
A major goal of bladder exstrophy (BE) surgery is to achieve micturating urinary continence or controlled dryness. This
study aims to quantify continence outcomes in classic BE managed using neonatal or delayed closure in a single
institution.
MATERIAL AND METHODS
Patients with classic BE were identified from the authors’ prospectively maintained database 1999-2015. The following
outcomes were measured: timing of closure (neonatal vs delayed), continence procedures (bladder neck repair, urinary
diversion), actual urinary continence according to a nationally agreed continence score (see below). Only patients 5
years of age or older were included in the study. Fisher’s Exact Test was used to compare the proportion of patients able
to void per urethra in each group, with P<0.05 considered significant.
RESULTS
Forty seven patients with classic bladder exstrophy were identified. 35 are voiding urethrally, 11 perform intermittent
self-catheterisation, 10 underwent bladder neck reconstruction; 12 patients required a continent diversion. Of the 35
patients voiding per urethra, 7 remain wet (Score 0), 10 have dry intervals but still required protection (Score 1), 5 are
dry during the day but wet at night (Score 2), 16 are dry day and night (Score 3), 1 is dry during the night but wet
during the day (Score 4). 15/25 and 13/22 patients respectively in the neonatal and the delayed group demonstrated a
continence score between 1 and 4 (P=0.592).
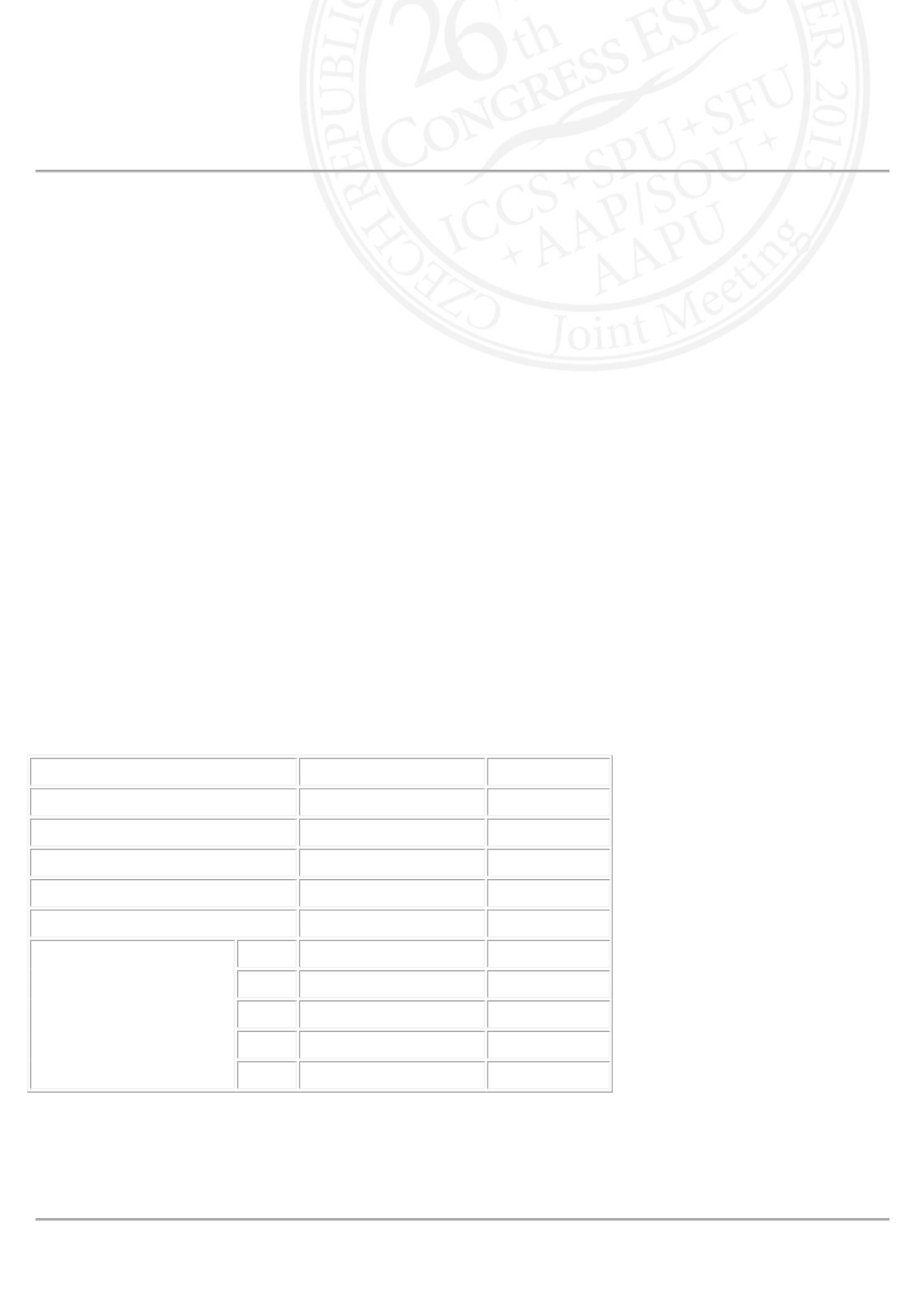
Primary neonatal closure Delayed closure
Number
25
22
Mean age (SD) years
11 (2)
7 (1)
Bladder neck reconstruction
6
4
Intermittent urethral catheterisation 8
3
Continent diversion
7
5
Continence Score
0
3/18
4/17
1
2/18
8/17
2
4/18
1/17
3
9/18
3/17
4
0/18
1/17
CONCLUSIONS
In the authors’ experience, delaying exstrophy closure has so far not resulted in a different proportion of patients
achieving urinary continence compared to neonatal closure. Longer follow-up may alter the findings of this study.












