
S4-16
(P)
VOIDING CYSTOURETROGRAPHY AFTER SURGICAL TREATMENT OF
VESICOURETERAL REFLUX: REWARDING OR PUNISHING?
Serhat GÜROCAK
1
, özgür TAN
1
, Cenk ACAR
2
, Iyimser ÜRE
3
, Irfan ATAY
1
, Esat AK
1
and Zafer SINIK
4
1) Gazi University Faculty of Medicine, Urology, Ankara, TURKEY - 2) Acibadem University Faculty of Medicine, Urology,
Istanbul, TURKEY - 3) Osmangazi university faculty of medicine, Urology, Eskisehir, TURKEY - 4) Pamukkale University
Faculty of Medicine, Urology, Denizli, TURKEY
PURPOSE
To investigate the usefulness of postoperative voiding cystouretrography(VCUG) in daily clinical practice after
endoscopic subureteral injection and ureteral re-implantation for vesicoureteral reflux.
MATERIAL AND METHODS
The records of the patients who underwent endoscopic subureteral injection and ureteral re-implantation for
vesicoureteral reflux at two academic centers were reviewed between 2009-2012. The patients were classified as low,
moderate and high-risk groups according to EAU paediatric urology guideline by using VCUG grade, presence of kidney
abnormality, lower urinary tract symptoms and toilet training. Postoperative clinical course, causes of failure,
intervention type, presence of postoperative VCUG were analyzed.
RESULTS
Surgical interventions were performed on 232 renal units(RU) in 159 patients. Mean age of the children was 6.78±5.5
years. 46(19.8%)RU’s were grouped as low-risk, 144 (62.1%) RU’s were moderate risk and 42(18.1%)RU’s were high-
risk. Distribution of postoperative VCUG and presence of urinary tract infection(UTI) were listed in table 1. In moderate
risk group who received subureteral injection; out of 57 RU’s, 5(8.8%)RUs had UTI. Among these, only 1(1.7%)
refluxing RU had UTI(p=0,880). In high risk group, out of 10 RU’s who received VCUG, 1(10%)RU had both reflux and
UTI(p=0,197). In re-implantation group, out of 37RU’s, only 1(%)RU had UTI without reflux.
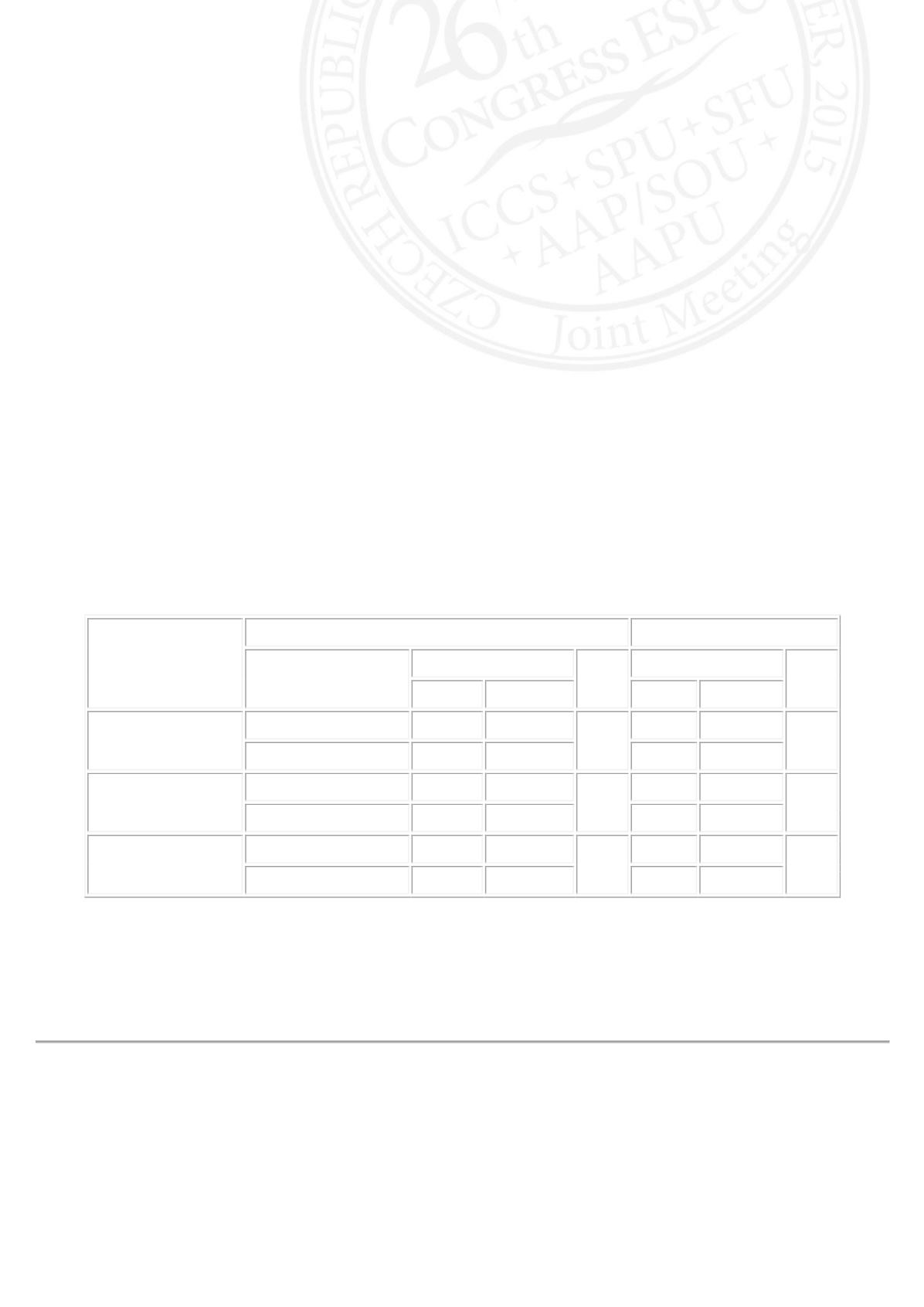
EAU guideline
Risk grouping
Injection
Ureteral Reimplantation
UTI
P
UTI
P
Positive Negative
Positive Negative
Low risk Group
Postop.VCUGpositive 1(%8.3) 11(%91.7)
0,768
Postop.VCUGnegative 2(%5.9) 32(%94.1)
Moderate risk Group
Postop.VCUGpositive 5(%8.8) 52(%91.2)
0,519
1(%20) 4(%80)
0,097
Postop.VCUGnegative 4(%5.8) 65(%94.2)
0
13(%100)
High Risk Group
Postop.VCUGpositive 1(%10) 9(%90)
0,244
0
7(%100)
Postop.VCUGnegative 0
13(%100)
0
12(%100)
CONCLUSIONS
The application of VCUG for postoperative evaluation didn’t give an extra clue to identify those patients at risk of further
surgical intervention in both groups. The results showed that follow-up after surgical intervention might be set on clinical
outcomes rather than VCUG.












