
14:24 - 14:28
ICCS S1-5
(SO)
OVERACTIVE BLADDER IN CHILDREN: ASSOCIATED SYMPTOMS AND FINAL
DIAGNOSIS
Jason VAN BATAVIA
1
, Angela FAST
1
, Andrew COMBS
2
and Kenneth GLASSBERG
3
1) Columbia University Medical Center, New York-Presbyterian Hospital, Urology, New York, USA - 2) Weill Cornell
Medical College, Cornell University, Urology, New York, USA - 3) Columbia University, Urology, New York, USA
PURPOSE
The ICCS defines OAB by the subjective symptom of urgency; DO is only implied. While no other symptom is required,
OAB can also be associated with urinary frequency, decreased functional bladder capacity, and incontinence. We sought
to determine how often these associated findings occur in OAB.
MATERIAL AND METHODS
The charts of 548 children (231M,318F; mean age 9.0, range 3-20) who presented sequentially with urgency (OAB)
were reviewed along with their final urodynamically-defined diagnosis which included dysfunctional voiding (DV),
idiopathic detrusor overactivity disorder (IDOD; ie, OAB with a short EMG lag time and quiet pelvic floor EMG during
voiding), detrusor underutilization disorder (DUD, similar to willful retention), and primary bladder neck dysfunction
(PBND).
RESULTS
Daytime incontinence was reported in 398 (72.6%) and frequency in 258 (47.1%). Mean %EBC was 80.9. (Table1).
Females were more likely to report daytime incontinence (76.7% vs. 67.5%,p=0.02) and frequency was found more
often in males (63.7% vs. 38.1%, p<0.001). %EBC was less in males (70.0 vs. 88.8, p<0.001). Table2 illustrates the
final diagnoses in patients presenting with urgency.
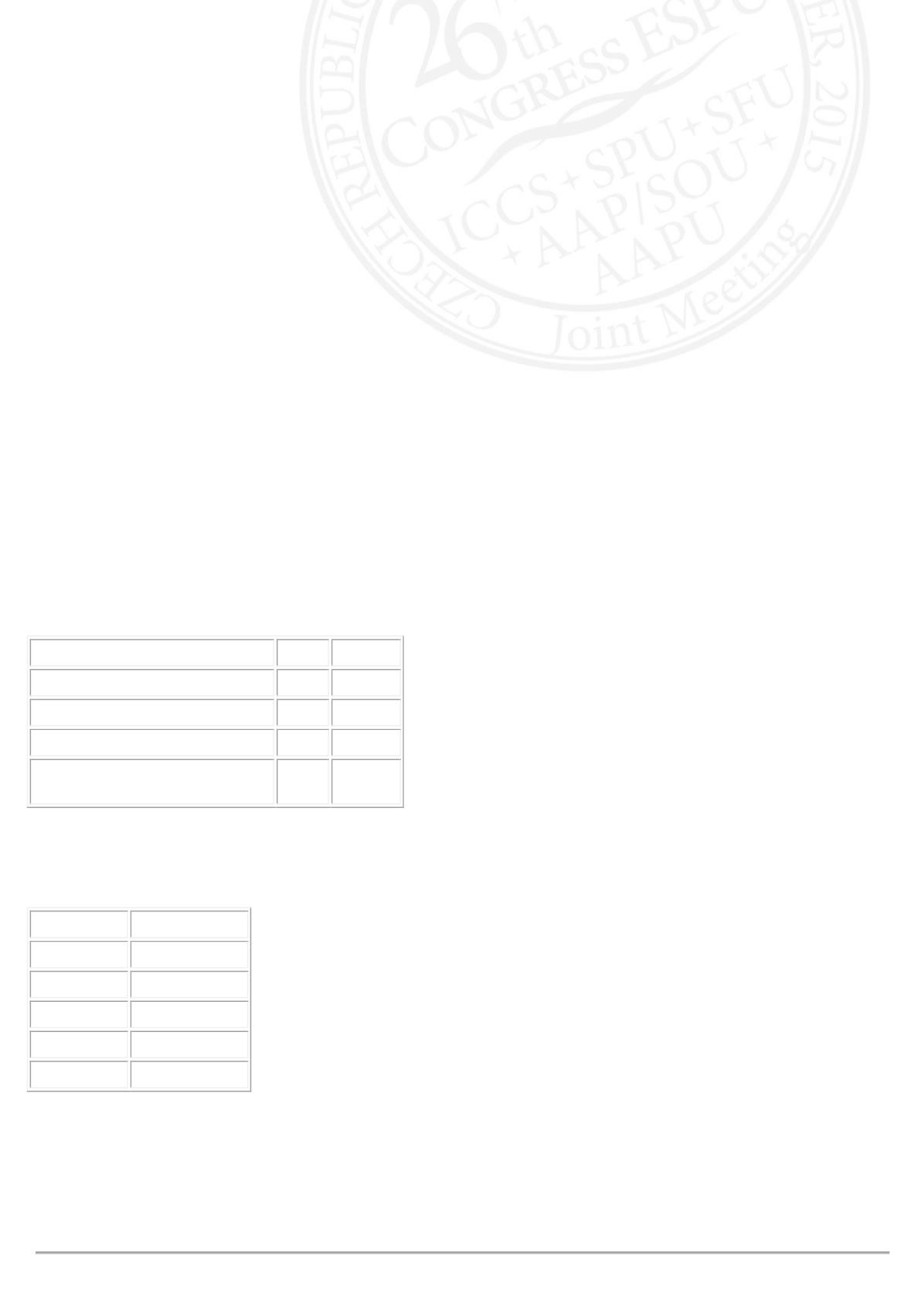
Table1. %EBC
Additional Symptom(s)
%EBC P-value*
Urgency alone(n=53)
117.2
With frequency(n=97)
82.7 <0.001
With daytime incontinence(n=237) 81.9 0.002
With frequency and daytime
incontinence(n=161)
65.9 <0.001
*=As compared to urgency alone
Table2. LUT condition diagnosis
Diagnosis
No. Patients(%)
DV
80(14.6)
IDOD
339(61.7)
DUD
16(2.9)
PBND
29(5.3)
None (OAB?)
85(15.5)
CONCLUSIONS
%EBC for age is usually normal or mildly increased in OAB when urgency is the only symptom but decreases
dramatically with each additional LUTS. OAB is more common in girls who also have a lower incidence of frequency,
more incontinence. and >%EBC. While the majority of children with OAB are diagnosed with IDOD, almost 15% will be
diagnosed with DV and another 5% with PBND.












