
ICCS S1-9
(P)
DIFFERENCE IN PATIENT AND PARENTAL RECOGNITION FOR LOWER URINARY
TRACT SYMPTOMS THROUGH CROSS-CULTURAL VALIDATED ADAPTATION OF
DYSFUNCTIONAL VOIDING SYMPTOM SCORE (DVSS) TO JAPANESE LANGUAGE.
Masaaki IMAMURA
1
, Akihiro KANEMATSU
2
, Tomoko USUI
3
, Kazuyoshi JOHNIN
4
, Koji YOSHIMURA
5
and Osamu OGAWA
5
1) Japanese Red Cross Otsu Hospital, Department of Urology, Otsu, JAPAN - 2) Hyogo College of Medicine, Department
of Urology, Nishinomiya, JAPAN - 3) Otemon Gakuin University, Faculty of International Liberal Arts, Department of
English Communication, Ibaraki, JAPAN - 4) Shiga University of Medical Science, Department of Urology, Otsu, JAPAN -
5) Kyoto University, Graduate School of Medicine, Department of Urology, Kyoto, JAPAN
PURPOSE
In using questionnaires for children with daytime incontinence (DI) or nocturnal enuresis (NE), it is unclear whether
children and parents respond to a question in the same manner. We performed cross-cultural validated adaptation of
Dysfunctional Voiding Symptom Score (DVSS, Farhat W et al. J Urol. 2000; 164: 1011-5) to a non-English language,
and evaluated patient and parental recognition.
MATERIAL AND METHODS
(1) Validation process. We translated DVSS into two non-English versions; pDVSS for parents and cDVSS for children.
Pre-testing was done with 5 to15-year-old patients by a specialist in cognitive linguistics. When a child needed help by
parents to understand a question, it was defined as ‘misidentification’. (2) Trial with children and parents. After we
completed the validated translation by amending the issues raised above, cDVSS or pDVSS were answered by children
or parents, respectively.
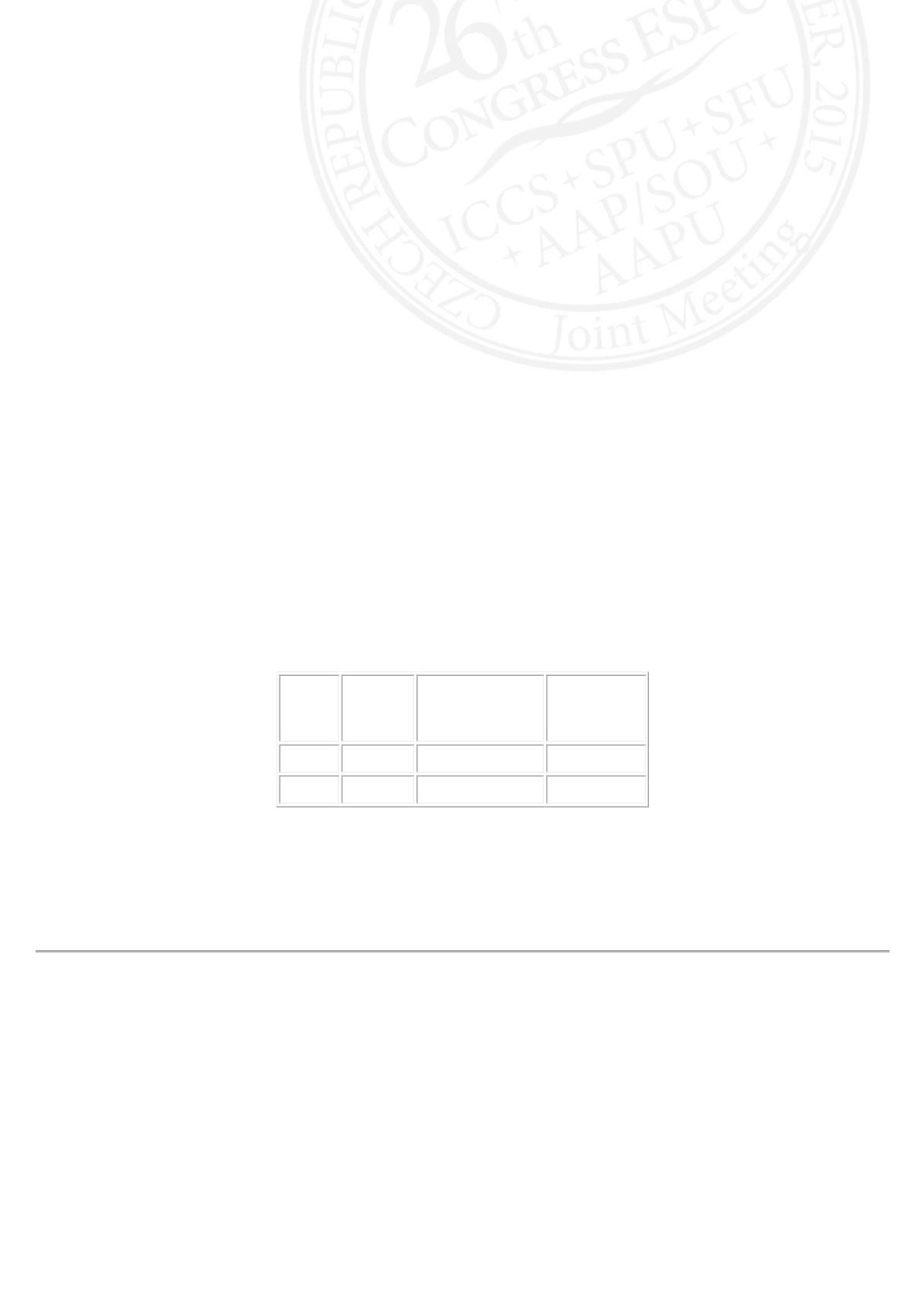
RESULTS
(1) Pre-testing was done for 32 patients. In children, a similar pattern of misidentification was observed for
representation of time or frequency. (2) There were 37 patients without DI or NE (control, Group 1), 35 with NE without
DI (Group 2), 29 with both DI and NE (Group 3). Group 3 showed significantly higher scores of DVSS than Group 1,
without discrepancy between cDVSS and pDVSS (Table, *compared to group 1). However, total scores and scores in
questions about bowel symptoms were significantly higher in cDVSS than in pDVSS (Table,
#
compared to pDVSS).
Group 1
(control)
Group 2
(NE without DI)
Group 3
(NE with DI)
cDVSS 3.9±3.1
3.1±2.6
#
8.3±3.5
*
pDVSS 3.4±3.0
2.3±2.7
7.4±3.9
*
CONCLUSIONS
Caution should be taken for using the terms related with time or frequency since temporal sense is not fully developed
in children. DVSS is useful for differentiating DI patients and control, but parents of NE without DI may under-estimate
bladder and bowel symptoms.












