
ICCS S1-11
(P)
INCIDENCE OF TOWER AND OTHER UROFLOW PATTERNS IN SHORT LAG TIME
PROVEN IDIOPATHIC DETRUSOR OVERACTIVITY (IDO)
Jason VAN BATAVIA
1
, Andrew COMBS
2
and Kenneth GLASSBERG
3
1) Columbia University Medical Center, New York-Presbyterian Hospital, Urology, New York, USA - 2) Weill Cornell
Medical College, Cornell University, Urology, New York, USA - 3) Columbia University, Urology, New York, USA
PURPOSE
In children with LUTS, uroflow patterns and EMG lag time are often used to support diagnoses. For instance, a tower
uroflow pattern (left shifted explosive curve) is thought to be indicative of idiopathic detrusor overactivity (IDO)
especially when associated with urgency. An EMG lag time of 0 seconds or less on uroflow/EMG has been shown to be
diagnostic of DO in children with LUTS. We sought to determine the spectrum of uroflow patterns, including tower
pattern, at presentation in children diagnosed with IDO by a very short EMG lag time and a quiet EMG during voiding.
MATERIAL AND METHODS
Only children diagnosed with IDO on the basis of a very short EMG lag time (ie, 0 seconds or less) and a quiet EMG
during voiding, on at least 2 studies, were included. Presenting LUTS and ICCS-described uroflow patterns were
reviewed
RESULTS
82 consecutive children (46M,36F; mean age 7.4 years, range 4-16) diagnosed with IDO were identified. Initial uroflow
patterns are shown in table 1. Only 9 patients (11%) had an initial tower flow pattern. Patients with tower flow were
more likely to have frequency, urgency, and daytime incontinence compared with children with other flow patterns (67%
vs. 49%, respectively, p>0.05).
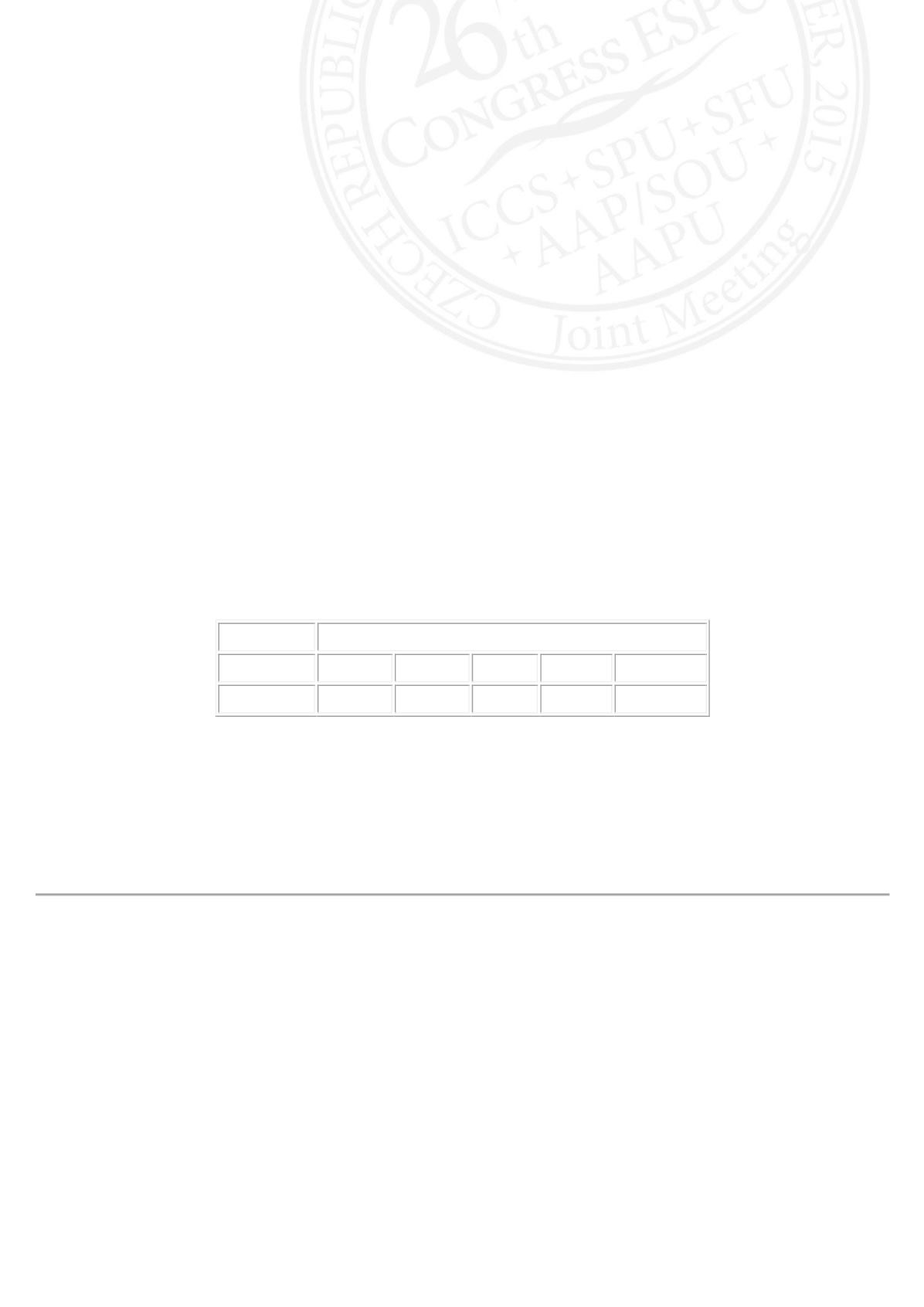
Table 1 Uroflow patterns at initial flow/EMG.
Uroflow Pattern
No. Patients Normal Plateau Tower Staccato Interrupted
82
46(56%) 17(21%) 9(11%) 8(10%)
2(2%)
CONCLUSIONS
Most children with IDO as evidenced by a very short EMG lag time and a quiet EMG during voiding do not exhibit a tower
uroflow pattern. Although not statistically significant, those with a tower pattern appeared to be the most symptomatic.
While a normal uroflow pattern was most common with IDO, 33% had flow curves often thought reflective of other LUT
conditions, supporting a cautionary note when relying on specific flow patterns alone to diagnose an underlying
condition.












